ChristianaCare has been a top-rated academic medical center for more than a century. Our residents and fellows experience a rigorous and rewarding combination of academic training and hands-on experience.
The Internal Medicine Residency Program attracts candidates from around the country who value our challenging university-affiliated academic curriculum within a community-based setting.
Our diverse patient mix offers residents exceptional opportunities to diagnose and treat a broad spectrum of primary-care diseases, as well as tertiary-care medical conditions not routinely encountered in smaller hospital settings.
ChristianaCare appoints 13 residents to the categorical internal medicine program each year. Additionally, ChristianaCare appoints 5 internal Medicine/Pediatrics and 3 Internal Medicine/Emergency Medicine interns each year.
Innovative training blocks
The ChristianaCare Internal Medicine Residency was the first program in the country to develop an innovative 4+2 ambulatory block schedule. Each resident’s schedule consists of a 4-week inpatient-medicine experience alternating with a two-week ambulatory-medicine experience.
The inpatient-medicine experiences will consist of general inpatient medicine at Christiana Hospital and Wilmington Hospital, as well as rotations in the MICU and CICU. Additionally, the inpatient based specialty rotations will occur during the 4-week blocks of time (e.g. cardiology, pulmonary, nephrology, hematology, infectious diseases and neurology). Each resident will have a half day of didactics weekly at our protected inpatient academic half day.
During each 2-week ambulatory block, residents will spend two full days per week in their outpatient continuity practice at Wilmington Hospital. In addition, each resident will have a half day per week of administrative time to work on research, performance improvement, or other patient care needs, and a half day of didactics weekly at our protected outpatient academic half day. The remaining four days over the 2-week block will be spent on subspecialty experiences. Time is available in the schedule to allow residents to tailor the curriculum to their individual learning needs and career goals.
Teacher-Manager-Learner
The inpatient medicine experience has adopted a “Teacher-Manager-Learner” model. As “Learners”, PGY-1 residents do just that- learn. Under the supervision of a PGY-3 resident and an attending physician they broadly build their knowledge in patient care, medical knowledge, communication skills, and professionalism. Our “Manager” teams allow PGY-2 residents to work side by side with an attending physician which provides greater autonomy. In addition to building on the knowledge they developed as “Learners”, “Managers” develop skills and knowledge in evidence based medicine, cost effective care, transitions of care, and working in a multidisciplinary team. Finally, we consider our PGY-3 residents “Teachers” and we provide them the autonomy to lead the team in making medical decisions. Perhaps more importantly we expect them to educate PGY-1 “Learners” (as well as 3rd and 4th year medical students), and role model the skills, knowledge, and attitudes they have developed during their first two years of residency training. We believe this graduated learning experience builds competency and confidence in our residents to become excellent physicians.
Program highlights:
- A challenging academic curriculum in a supportive, collegial environment
- Inpatient rotations in a 1000+ bed Level 1 trauma center and tertiary referral center with incredible patient diversity and breadth of pathology
- Two training facilities offering suburban and urban training experiences
- Excellent placement for our residents in competitive fellowships and post-residency jobs
- On-site fellowships in cardiology, interventional cardiology, hematology & oncology, hospice & palliative medicine, sports medicine, and clinical informatics
- Outstanding scholarly opportunities in original research and quality improvement
- Residencies in Categorical Internal Medicine, Combined Medicine/Pediatrics, and Combined Internal Medicine/Emergency Medicine
Other unique features
- Largest teaching affiliate of Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia and branch campus site for the Philadelphia College of Osteopathic Medicine
- State-of-the art 9,000 square foot simulation center
- Optional global health experiences, resident research training program, advanced quality improvement elective, and leadership training opportunities
- As the largest health system in Delaware, we are in invested in the health of our state and our community
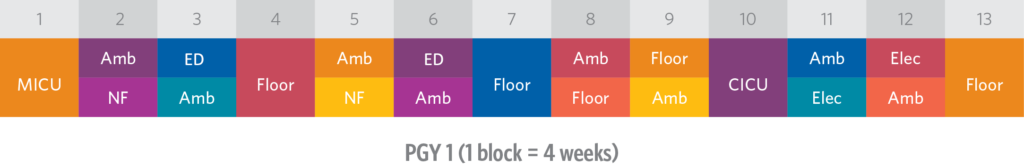
Sample PGY-1 block schedule
Sample ambulatory schedule
| Monday | Outpatient Continuity |
|---|---|
| Tuesday | Subspecialty Outpatient |
| Wednesday | Outpatient Continuity/Admin |
| Thursday | Academic Half Day/Continuity |
| Friday | Subspecialty Outpatient |
Night float
We have a fully integrated night float system on every inpatient rotation. Interns do an average of four weeks of inpatient floor night float and two weeks of ICU night float during the first year. Interns on inpatient rotations share “short call” (until 7:00pm) responsibilities and on average have one of these shifts every three to four days.
A resident’s typical day
| Inpatient Floor Services (on a non-didactic workday) | ||
|---|---|---|
| 0600 – 0630 | Start time. Obtain sign in from on-call team. Critical patients are to be seen immediately | |
| 0700 – 0900 | Interns evaluate patients and write progress notes | |
| 0900 – Noon | Work Rounds with the team | |
| 1300 – 1630 | Admissions, chart reviews, etc. | |
| 1700 – 1800 | Sign out. New admissions are reviewed, and potential problems are identified | |
| Intensive Care Units (on a non-didactic workday) | ||
| 0600 – 0630 | “Start time.” Obtain sign in from on-call team | |
| 0730 – 0930 | Work Rounds. Interns and residents evaluate patients, write notes, and order tests | |
| 0930 – Noon | Teaching Attending Rounds | |
| 1300- 1600 | Admissions, chart reviews, etc. | |
| 1600 – 1700 | Sign-Out. All patients are reviewed, and potential problems are identified | |